 |
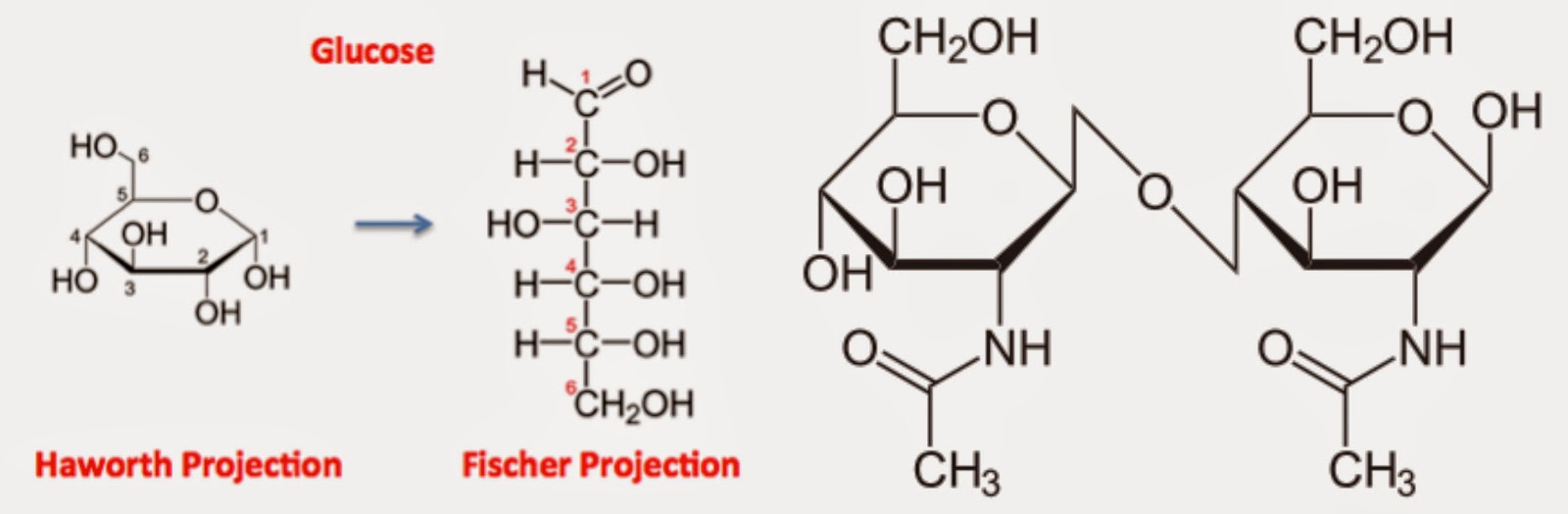
| Example of a monosaccharide on the left, and disaccharide on the left, which is 2 monosaccharides linked together by an oxygen. |
Larger carbohydrate chains that are made up of 3-10 simple sugars (i.e. monosaccharides), are known as oligosaccharides, and are abundant in various foods including asparagus, onion, artichoke, legumes, wheat, and garlic. Last but not least, there are polyols, which are sugar alcohols, or common sugar-free substitutes, including xylitol and sorbitol, while they are also found in real food sources such as grapes, mushrooms, avocado, apricots, and many others.
Why it Matters
Overall, the main takeaway from these differing types of carbohydrates found in food, is that the bodies small intestine has a hard time digesting them. In fact, this is even true for those that are completely healthy. Therefore, when the food that enters the small intestine is unable to be broken down, it remains so when it enters into the large intestine, where it then feeds gut bacteria. Though having happy gut bacteria is important to obtaining a balanced GI tract, over-feeding them causes the microbes to become over-active, fermenting everything that they can get their “hands” on. In turn, this causes one to have a variety of symptoms that can range from minor discomfort in one’s abdomen, to inhumane, debilitating pain throughout one’s entire body. Not only does undigested food in the small intestine cause overgrowth (i.e. SIBO), but it also hinders the large intestine from its key job (water absorption), which is why bloating, bowel issues (constipation and, or, diarrhea), gas, cramps, indigestion, and belching, are all common symptoms of FODMAP intolerance as well. Enterocyte cells, as mentioned in my previous, leaky gut post here, are one of the major factors in the health status of one’s gut, and are also responsible for digesting many FODMAPs. Therefore, if they become damaged or dysfunctional, not only does allergies and other inflammatory health conditions come as a result, but also the chance of FODMAP intolerance and overgrowth. Common triggers of GI damage include gluten, medications (antibiotics, NSAIDs, birth control, etc…), alcohol, legumes, and other items prominent in the SAD (standard American diet), all of which lead to a a leaky gut, which, as mentioned above, subsequently adds to the likely hood of one becoming noticeably FODMAP intolerant. FODMAP intolerance can also occur when the expression of Glucose Transport Protein 5 present in the GI tract, becomes dysfunctional, due to it being one of the main fructose transporters in the body. This cant occur through ingestion of polyols and sugar alochols, due to their direct effect on the function of GLUT5. As Dr. Sarah Ballantyne mentions in her post, what type of FODMAP one adversely reacts to, can sometimes be brought back to what insufficiency is occuring in the body, with fructose and polyols being related to GLUT5 deficiency, and fructan containing foods, being from a lack of certain digestive enzymes.
How to Heal
If intolerance to FODMAPs is caused by a damaged gut, then it is quite obvious that one of the only ways to fully reverse this is to first begin to heal one’s gut. For starters, it is important to eliminate, or at least decrease (depending on the extent of one’s intolerance), the amount of dietary sources of fermentable carbohydrates in one’s dietary intake, as well as other foods, medications, and substances that have a negative impact on gut health. This can take anywhere from a few weeks, to months, or even years, depending on the degree of one’s health condition. It is also key to get one’s gut flora balanced, of which can be done through supplemental probiotics, or probiotic foods. However, one must be careful while introducing more bacteria to the gut when experiencing FODMAP intolerance, as it may make their symptoms progressively worse. Truly, it depends on the person, and what is the underlying cause of their gut imbalance. Below is a brief list of foods high in FODMAPs, however, if you are looking for more information on both gut healing and the information discussed today, I encourage you to purchase Dr. Sarah Ballantyne’s, “The Paleo Approach,” or visit the various resources provided at the end of this post.
The Paleo Approach
Ballantyne, Sarah. The Paleo Approach: Reverse Autoimmune Disease and Heal Your Body. N.p.: n.p., n.d. Print

Thank you for this post Gabriella, and thank you for sharing the rough details of your journey. I’m so sorry that you’ve experienced so much suffering and frustration with your health! Your grit and ‘fight’ as you face your challenges is very inspiring to me, and encourages me to also fight and keep trying things “that might help” as I face a maddening journey of “maybes” and question marks. I’m praying that your journey absolutely comes to a point of health and wellness and calm waters. Thank you for helping others find better health even as you continue to battle. ~~
Hi, do you eat snacks? I’ve ear that it’s better to avoid snacking if you suffer of SIBO but I’m not sure what’s it’s the best.
Thank you.
I do not eat snacks…They pretty much wreck havoc on my gut in-between meals. I typically aim for 4 hours in-between meals at least.
Hello Gabriella. I admire all of the strength you have for what you have had to go through. My 17 year old daughter is going through this now. After seeing over 15 doctors, we will be seeing a Lyme doctor in a week. She too was diagnosed with Leaky Gut. She did the SIBO test as well. According to the gastro doctors, she did not have it. However, the holistic doctor said that the guidelines have changed in the last month so in fact she does have it. My question to you—did the doctors try to heal the gut first with the anti inflammatory diet and then the SIBO diet, or what? That is where we are now. She has lost 15 pounds on the anti inflammatory diet. Also, who is your lyme doctor that is treating you>
Thank you so much.
Kelli
Hi Kelli,
My heart goes out to you and your daughter…As far as the SIBO aspect, I put myself on the SIBO diet first, though it was naturally AIP in nature (if that is what you mean by anti-inflammatory?). I find that whenever my infections ramp up really bad, losing weight is inevitable, though the key for me is just keeping my fat intake high so that my body has something to run off of since my GI tract cannot handle starchy veggies and such. My doctor who treated me for SIBO is Dr. Leo Galland.
Hello, I was thinking to incorporate hydrolyzed collagen and gelatin to my diet to help with leaky gut.
I’m also doing a combination of SCD + FODMAP … but I read that bone broth can have polysaccharides so maybe I shouldn’t add these supplements, What do you think? Thanks for your huge help.
Hello Conchi,
From what I have experienced the FODMAPs in bone broth are from the garlic,onion, and celery commonly used. Cartilage bones are also supposedly high in FODMAPs, which is why I use marrow bones to make my bone broth. The Paleo Pi has great, short summary of this info if you haven’t seen it already (http://thepaleopi.com/2015/01/23/bone-broth-gelatin-bloating/). I personally do not do well with drinking bone broth, though I believe it to be histamine related since I have a serious mast cell disorder. The hydrolyzed collagen by Vital Proteins has been the friendliest to my gut and all its complications so far…Hope this helps!
Thank you!
We’ll see if my bacteria also think that’s a good idea haha.
Gabriella, happy new year!
Can I ask you if probiotics have helped you to increase your levels of good bacteria?
I have seen many people that say that, despite taking probiotics,they have zero good bacteria(stool test).
hmm, it seems complicated to change the microbiome.
Thank you!
Your story really resonated with me. I’m early in my journey with treating long-term Lyme (among other things) and struggle with bouts of ischemic colitis due to one offline intestinal artery and another intestinal artery compressed by a diaphragmatic ligament (leaving me with only one properly working one, which is unfortunately compromised by chronic anemia from losing 40% of the blood in my body every few weeks…). I’m also dealing with intermittent intestinal paralysis and mild leaky gut. I’ve never anyone who had so much overlap with the things I’m dealing with. I mention that in part as an apology for asking a question for which I imagine the answer is already present somewhere in your generous blog (since I’m pretty wiped out and easily confused and don’t know where to look right now): How are you doing now? Which things have made the biggest difference for you with the Lyme and intestinal issues?